There are a lot of factors to all this, but here are the basics. I’ve been traveling, staying in hotels for about a week, and fasting for three days before travel, then following ketosis levels for a week during travel. I usually get a lift as I hit ketosis, with Heart Rate Variability(HRV), cortisol levels, stress, sleep, etc., all showing very positive effects. But if I push ketosis levels too much, I experience negative effects, and all these factors slide massively. I tried to push through, with ketones over 3mmol/L for a consistent week. I didn’t lose weight, felt worse, and slept horribly.
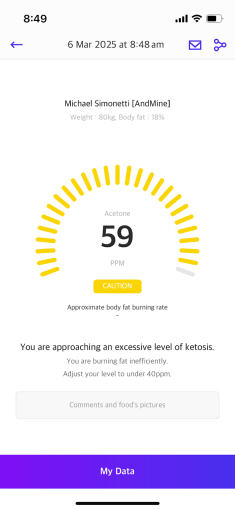
Ketoacidosis? Possibly for a day… I had a 60+ reading, maybe 5mmol/L, a few times on KETOSCAN (concerning) and switched to SIBIO CKM to figure out this metabolic stress problem. The question remains: is stress BAD? Obviously, with elevated cortisol levels in my system, I also had higher glucose even though I was eating ZERO carbs.
The Pre-Testing Phase: Uncovering the Impact of Fat Metabolism, Cortisol Levels, and Poor Sleep
For about a week leading up to my recent metabolic adjustments, I experienced a period of heightened stress, poor sleep quality, and physiological strain. My Garmin data consistently showed elevated nighttime stress levels, suppressed heart rate variability (HRV), and overall lower recovery scores. At first, I suspected an isolated dietary issue—primarily related to dietary fat intake—but a deeper analysis revealed multiple contributing factors.
Key Factors Affecting Ketosis Levels and Metabolic Stress
Fat Overload & Free Fatty Acid (FFA) Accumulation: Even on days when I didn’t significantly overconsume dietary fat, my body remained in a heightened stress state, suggesting that previous fat metabolism issues may have had lingering metabolic effects.
Cumulative Stress Load: Travel, poor sleep, and overextending myself with too many tasks contributed to systemic stress, keeping my body in a prolonged fight-or-flight mode.
Fasting Ketosis & Cortisol Levels Interaction: While fasting ketosis generally improves metabolic flexibility, in this scenario, it may have exacerbated cortisol levels, further suppressing HRV and increasing overnight stress.
Persistent Gluconeogenesis: My glucose levels hovered slightly elevated (around 7 mmol/L), while ketones remained relatively stable at ~2 mmol/L, indicating that elevated cortisol levels were likely driving gluconeogenesis rather than a smooth metabolic balance.
Through this phase, I recognized that overloading my system wasn’t just about dietary fat intake; it was also about how multiple stressors—both physical and psychological—layered on top of each other, creating an environment of persistent metabolic stress.
Key Learnings on Ketosis, Cortisol Levels, and Fat Metabolism
Metabolic stress is multifactorial: Dietary fat intake is just one piece of the puzzle; lifestyle factors like travel, workload, and poor sleep can amplify its effects.
HRV and stress tracking are essential: Real-time data from my Garmin provided early indicators that something was off, even before I felt it physically.
Cortisol levels play a major role in metabolic balance: Extended fasting ketosis or excessive fat metabolism in a high-stress state can drive gluconeogenesis, potentially keeping glucose elevated.
One key observation was that even on days when I didn’t significantly overload dietary fat, my body remained in a state of heightened metabolic stress. This indicated that while fat metabolism played a role, external stressors such as travel, poor sleep, and an overextended schedule were amplifying the effect. The cumulative impact of these stressors likely created a scenario where my body was unable to efficiently clear excess free fatty acids (FFAs), leading to sustained metabolic stress.
Additionally, fasting ketosis—normally a tool I use effectively for metabolic flexibility—may have inadvertently increased cortisol levels, further suppressing HRV. The combination of poor sleep and metabolic stress likely compounded the issue, keeping my body in an extended fight-or-flight state even during periods of rest. My glucose levels hovered slightly elevated (around 7 mmol/L), while ketones remained relatively stable at ~2 mmol/L, suggesting ongoing gluconeogenesis driven by stress rather than a smooth metabolic balance.
Through this phase, I recognized that overloading my system wasn’t just about dietary fat intake; it was also about how multiple stressors—both physical and psychological—layered on top of each other, creating an environment of persistent metabolic stress. This realization set the stage for deeper testing and adjustments to better align my fasting ketosis, diet, and recovery strategies with my body’s actual needs.
This realization set the stage for deeper testing and adjustments to better align my fasting ketosis, diet, and recovery strategies with my body’s actual needs.
For more health insights like this, visit our website today! BE US – Health is Wealth.
